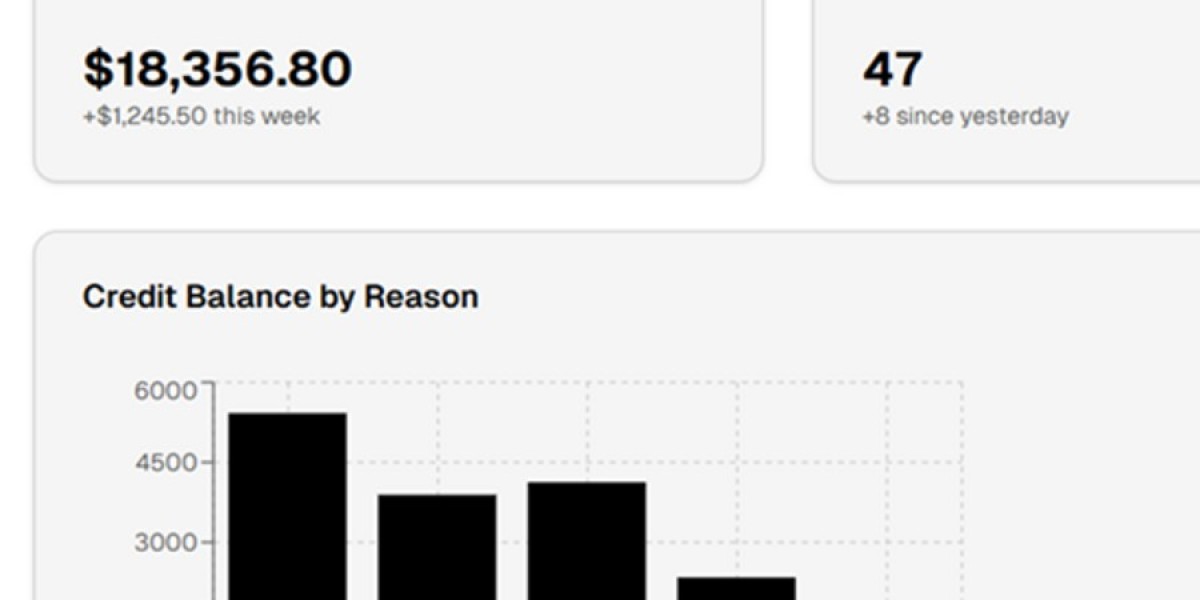
Credit Balance in Medical Billing: What Providers Need to Know
A credit balance in medical billing occurs when a payment exceeds the amount owed on a patient’s account. These overpayments may come from insurance payers, patients, or coordination of benefits errors. If not managed correctly, credit balances can lead to compliance issues, financial penalties, and revenue leakage.
Common Causes of Credit Balances
Duplicate insurance or patient payments
Incorrect charge entry or payment posting
Overpayments from insurance carriers
Reversed or adjusted claims not updated properly
Coordination of Benefits (COB) errors
Why Credit Balance Management Is Important
Unresolved credit balances can trigger audits, payer takebacks, or regulatory penalties. Healthcare providers are required to refund overpayments within a specific timeframe to remain compliant with payer and federal regulations.
Best Practices for Managing Credit Balances
Perform regular credit balance audits
Identify payer vs. patient overpayments accurately
Process refunds promptly and document actions
Implement strong payment posting and reconciliation processes
Use experienced billing professionals for resolution
Proper credit balance resolution in medical billing not only ensures compliance but also improves financial transparency and trust with patients and payers.