Meningitis is a serious medical condition characterized by inflammation of the meninges the protective membranes covering the brain and spinal cord. Because the central nervous system is involved, meningitis can rapidly become life-threatening if not diagnosed and treated promptly. Globally, it remains a significant cause of morbidity and mortality, particularly among infants, young children, immunocompromised individuals, and populations in resource-limited regions.
Understanding the causes and symptoms of meningitis is critical for early detection, timely intervention, and prevention of complications such as brain damage, hearing loss, or death.
What is Meningitis?
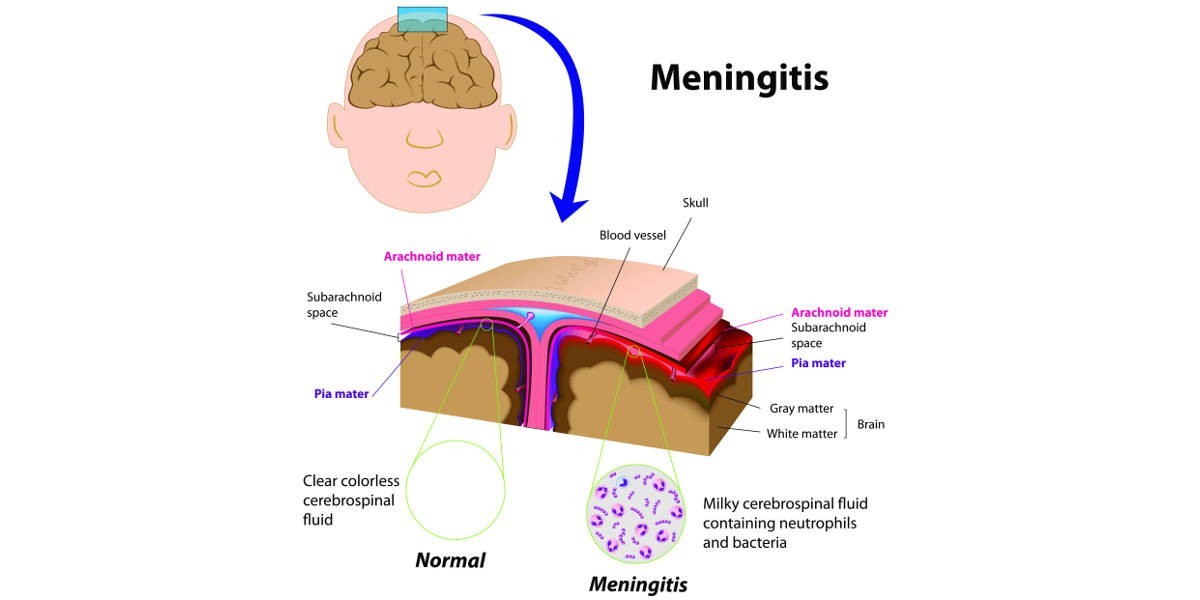
Meningitis refers to inflammation of the meninges, which consist of three layers:
Dura mater (outer layer)
Arachnoid mater (middle layer)
Pia mater (inner layer)
When infectious agents breach the blood-brain barrier or spread from nearby infections (such as sinusitis or otitis media), they can trigger an inflammatory response in these membranes. This inflammation increases intracranial pressure and disrupts normal neurological function.
Meningitis can be classified based on its etiology:
Bacterial meningitis
Viral meningitis
Fungal meningitis
Parasitic meningitis
Non-infectious (aseptic) meningitis
Among these, bacterial meningitis is the most severe and requires urgent antimicrobial therapy, often including third-generation cephalosporins such as ceftriaxone.
Causes of Meningitis
1. Bacterial Causes
Bacterial meningitis is the most dangerous form and can progress rapidly. The most common pathogens vary by age group and geographic location.
Key bacterial agents include:
Neisseria meningitidis
Streptococcus pneumoniae
Haemophilus influenzae
Listeria monocytogenes
Escherichia coli
Transmission typically occurs through respiratory droplets, close personal contact, or contaminated food (in the case of Listeria). In neonates, infection may occur during childbirth.
Because bacterial meningitis can deteriorate within hours, empirical intravenous antibiotics are initiated immediately after clinical suspicion. In many treatment protocols, ceftriaxone injection wholesale procurement is essential for hospitals, emergency units, and global health programs to ensure uninterrupted supply of this broad-spectrum antibiotic.
2. Viral Causes
Viral meningitis is generally less severe than bacterial meningitis and often resolves without specific antiviral treatment.
Common viral agents include:
Enterovirus
Herpes simplex virus
Varicella-zoster virus
Mumps virus
Enteroviruses are the most frequent cause, particularly in late summer and early autumn. Viral meningitis is sometimes referred to as aseptic meningitis.
3. Fungal Causes
Fungal meningitis is rare but more common in immunocompromised individuals, including those with HIV/AIDS or undergoing chemotherapy.
The most notable fungal cause is:
Cryptococcus neoformans
Fungal meningitis usually develops more slowly and requires long-term antifungal therapy.
4. Parasitic Causes
Parasitic meningitis is uncommon and may result from exposure to contaminated water or soil. Certain parasites can cause eosinophilic meningitis, a specific inflammatory response characterized by elevated eosinophils in cerebrospinal fluid.
5. Non-Infectious Causes
Non-infectious meningitis can result from:
Autoimmune diseases
Certain medications
Malignancies
Head injury or neurosurgery
This type is termed aseptic meningitis when no bacterial pathogen is identified.
Risk Factors for Meningitis
Several factors increase susceptibility:
Age (infants and elderly at higher risk)
Compromised immune system
Living in close quarters (dormitories, military barracks)
Lack of vaccination
Chronic medical conditions
Recent ear or sinus infection
Vaccination programs targeting pneumococcal, meningococcal, and Haemophilus influenzae type b infections have significantly reduced incidence in many countries.
Symptoms of Meningitis
The clinical presentation of meningitis depends on the causative organism, patient age, and disease severity. However, several hallmark symptoms are commonly observed.
Classic Triad
In bacterial meningitis, the classic triad includes:
Fever
Neck stiffness (nuchal rigidity)
Altered mental status
However, not all patients present with all three simultaneously.
Early Symptoms in Adults and Older Children
High fever
Severe headache
Stiff neck
Nausea and vomiting
Sensitivity to light (photophobia)
Confusion or difficulty concentrating
Seizures
A distinctive rash may occur in meningococcal meningitis caused by Neisseria meningitidis. This rash can progress rapidly and is considered a medical emergency.
Symptoms in Infants
Infants may exhibit non-specific signs, including:
Irritability
Poor feeding
Vomiting
Bulging fontanelle
Excessive sleepiness
High-pitched crying
Seizures
Because symptoms can be subtle, early medical evaluation is critical.
Advanced or Severe Symptoms
If untreated, meningitis can lead to:
Coma
Hearing loss
Cognitive impairment
Stroke
Septic shock
Death
The rapid progression of bacterial meningitis underscores the importance of immediate antibiotic therapy. In many healthcare systems, maintaining reliable ceftriaxone injection wholesale supply chains is vital to ensure that first-line empiric therapy is readily available in emergency settings.
Pathophysiology of Meningitis
The disease process generally follows these steps:
Colonization of mucosal surfaces
Invasion into the bloodstream
Crossing of the blood-brain barrier
Inflammatory response in the meninges
The inflammatory cascade releases cytokines and other mediators that increase vascular permeability, leading to cerebral edema and increased intracranial pressure. These mechanisms account for many neurological symptoms.
Diagnosis
Diagnosis typically involves:
Clinical examination
Blood cultures
Lumbar puncture (spinal tap)
Cerebrospinal fluid (CSF) analysis
Imaging (CT or MRI when indicated)
CSF findings differ depending on whether the cause is bacterial, viral, or fungal.
In suspected bacterial meningitis, treatment should begin immediately often before laboratory confirmation due to the risk of rapid deterioration.
Treatment Overview
Treatment depends on the underlying cause:
Bacterial meningitis: Immediate intravenous antibiotics (commonly ceftriaxone plus vancomycin), sometimes corticosteroids
Viral meningitis: Supportive care; antivirals for specific viruses
Fungal meningitis: Antifungal medications
Parasitic meningitis: Antiparasitic drugs
Ceftriaxone remains a cornerstone in empiric therapy because of its broad-spectrum activity and favorable pharmacokinetics. For hospitals, distributors, and public health programs, managing ceftriaxone injection wholesale logistics is a critical component of infectious disease preparedness.
Prevention
Preventive measures include:
Vaccination (meningococcal, pneumococcal, Hib vaccines)
Prophylactic antibiotics for close contacts of meningococcal cases
Good hygiene practices
Prompt treatment of ear and sinus infections
Public health initiatives have significantly reduced the global burden of meningitis, though outbreaks still occur, particularly in the African “meningitis belt.”
Conclusion
Meningitis is a potentially life-threatening condition characterized by inflammation of the meninges surrounding the brain and spinal cord. It can be caused by bacteria, viruses, fungi, parasites, or non-infectious conditions. Among these, bacterial meningitis is the most severe and requires urgent medical intervention.
Recognizing early symptoms such as fever, stiff neck, severe headache, and altered mental status is essential for rapid treatment. In infants, symptoms may be subtle but equally dangerous.
Timely diagnosis, appropriate antimicrobial therapy, vaccination, and strong pharmaceutical supply systems including reliable ceftriaxone injection wholesale distribution are all crucial in reducing mortality and long-term complications associated with meningitis.
Early medical attention saves lives. When meningitis is suspected, immediate evaluation and treatment are imperative to prevent devastating outcomes.